Your Trusted Partner in Mobile Rehabilitation
Physiotherapists are Rehabilitation Specialists. We are highly trained to manage your rehabilitation with concurrent medical issues. Our goal is to help you regain confident and independent movement, safely and effectively.
Physicare helps you with

Comfort and Convenience
We deliver quality physiotherapy rehabilitation to your home so you conserve energy and time
Peace of Mind
We are highly experienced in rehabilitation, from ICU to specialised rehab units to home
Muscle Strengthening
We teach strengthening of your postural muscles as well as the muscles that help you move

Pain Management
Our priority is to teach you to control your pain and trace and treat the source of your pain

Fascia Release
We use advanced dry needling techniques to release scar tissue and mobilise fascia
Joint Mobility
We teach you the stretches required to relieve your pain and to improve your biomechanics
What We Offer
Assessments
Therapy
Training
Conditions We Treat
Here are some of the ways we can help
Orthopaedic
Rehabilitation
After surgery to repair fractures, tendon or ligament or joint replacement surgery, you will need to undergo rehabilitation.
Physiotherapy Goals
To restore movement, strength and function of the affected joint in a safe progression, while respecting the healing process in the surgical/fracture site.
Techniques Used
Biomechanical Analysis
Point of Care Ultrasound
Dry Needling
Aids Prescription
Therapeutic Exercises
Gait Retraining
Musculoskeletal/Sports Rehabilitation
We treat muscle and joint dysfunction and pain in the neck, back, wrist, elbow, shoulder, hip, knee, ankle and foot.
Physiotherapy Goals
We assess to find the root cause of the pain and treat it. The goals of Physiotherapy are to reduce pain, restore functional movement and strength.
Techniques Used
Biomechanical Analysis
Postural Assessment
Point of Care Ultrasound
Shockwave Therapy
Clinical Pilates
Taping
Dry Needling
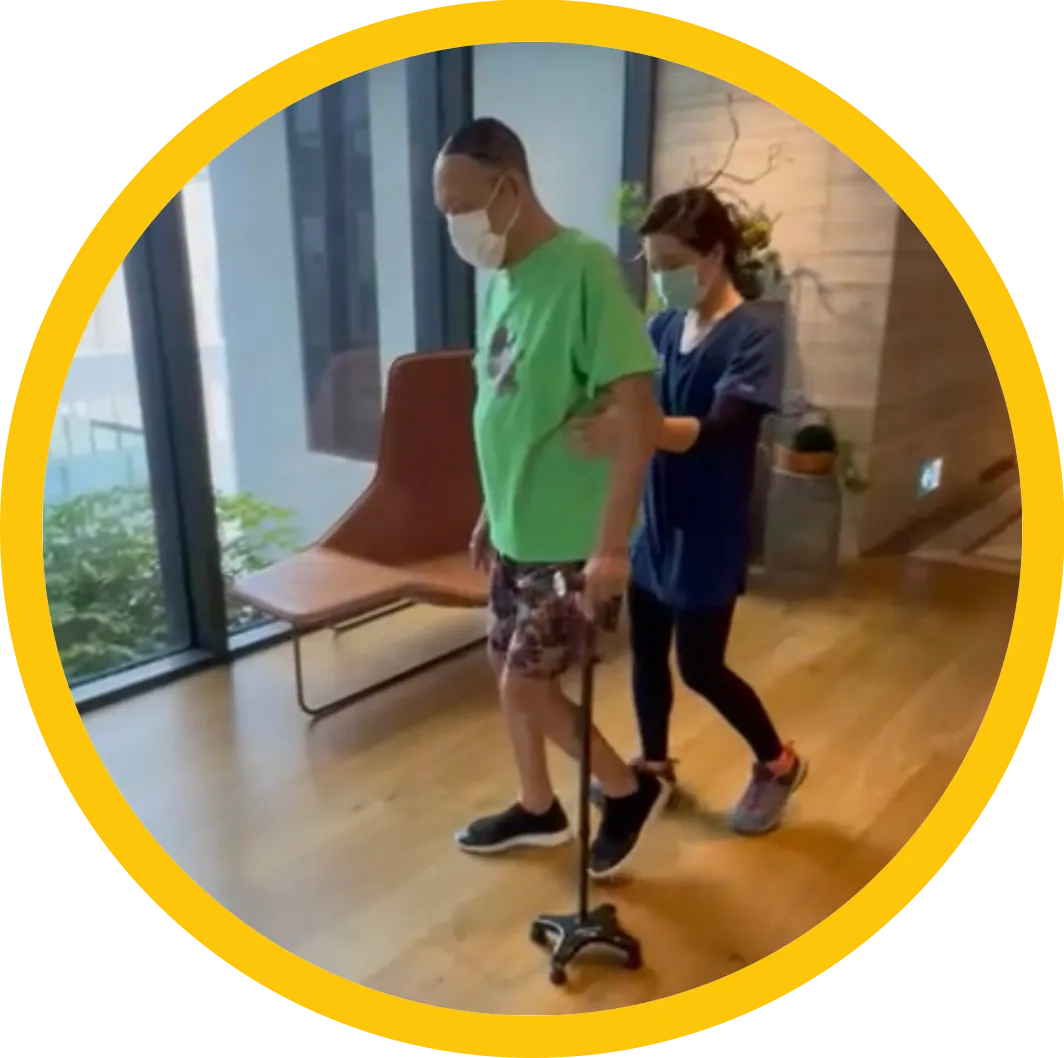
Neurological
Rehabilitation
Mild strokes can be managed at home by improving strength, sensation, balance and coordination.
Physiotherapy Goals
To forge new neural pathways within the brain by retraining the body to move functionally.
Techniques Used
Gait Analysis & Retraining
Principles of motor control Proprioceptive neuromuscular facilitation
Therapeutic Exercise
Aids Prescription
Chest
Physiotherapy
Poorly ventilated lungs result in poor blood oxygen levels, breathlessness and impedes movement
Physiotherapy Goals
To clear secretions from lungs to ensure efficient oxygen exchange, improve oxygen concentration levels and encourage movement.
Techniques Used
Percussion & Vibes
Postural Drainage
Ventilation Techniques
Active Cycle of Breathing
Realise your Rehabilitation Potential
Living in pain? Frustrated because you are not walking well? Get a thorough assessment to see what you can truly achieve with Physiotherapy, in the comfort and convenience of home.
REHABILITATE WITH CONFIDENCE

2 DECADES OF REHAB
We have experience in the whole rehabilitation spectrum and can accurately assess your rehabilitation potential. We are results driven to meet your goals quickly

TRULY MOBILE
We have treated patients all over the world. From Australia, the UK, Singapore, Jakarta and China. From hospitals, to homes and hotels, as well as on the sports field.

LONG TERM VISION
Your body is the most amazing thing you will ever own. Our treatment plans are designed to keep you strong now and into the future
Professional Registrations & Membership